Sleep. We all need it, but why is it such a struggle?
Professionals in occupational therapy call the basic habits and practices that enable us to sleep well on a day-to-day basis “sleep hygiene,” but trying to figure out why we don’t sleep or fall asleep well, is much harder than it sounds.
In addition, I am loving all the new research out there to address sleep, including using the PEOP model by using “occupation-based sleep intervention to focus on strategies to (1) minimize the influence of bodily function on sleep, (2) promote environment conducive to sleep, and (3) restructure daytime activity with a focus on occupational balance.”
In this post, I will share 8 tips to teach your patients sleep hygiene, as well as a free sleep questionnaire that you can print off and use to dig into the roles, habits and routines of sleep.
8 Tips to Address Sleep Hygiene in OT
1. What do you do to get ready for bed as part of your sleep hygiene?
Believe it or not, pre-bed routines are a real thing and can definitely affect sleep patterns. Having a daily routine such as reading before bed, brushing your teeth, changing your clothes, etc tells your internal clock you are about to go to bed.
Tip: Start a routine!
Try winding down with some quiet time before you go to sleep and avoid over-stimulation – because finishing up a stressful phone call, paying your bills or watching the news right before bed doesn’t let your body prepare you for hitting the hay.
2. How long does it take you to actually go to sleep and why?
30 minutes is pretty average for a person without a “sleep disorder,” but this varies from person to person. Consider things such as:
- Are you worried about something?
- Do you have a hard time turning your brain “off?”
Tip: Consider learning some deep breathing or meditation techniques to clear your mind.
• De-stress techniques to calm you down before bed will help you enter transitional sleep, which slows down your brain waves and helps begin the sleeping process.
3. How many hours do you get a night?
This number is variable – depending on your age. Recommended number of hours a night is 7-8.
Actually getting too much can actually be just as problematic as too little sleep!
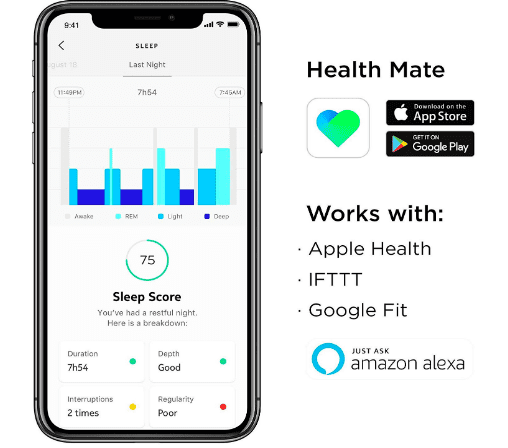
Tip: Sleep trackers will track how long you are actually sleeping at night and knowing your metrics can be key in sleep hygiene. It gives you a good idea if you are going into REM, or if you are constantly waking up throughout the night. Not only is this information can be valuable to figuring out the reason for insomnia, but if you keep track of it over a period of time, it will help determine if your quality of sleep has changed.
4. Are you able to stay asleep?
How many times do you wake up a night and why? Do you have sleep apnea? Do you have an overactive bladder and have to go to the bathroom? Are you a light sleeper and noises keeping you awake? Are you worried about something?
Think about why you can’t stay asleep and address it!
Tip: Stop drinking water or coffee 3-4 hours before going to sleep prevents people from waking up at night to go to the bathroom.
• Medical problems such as sleep apnea, an overactive bladder or incontinence are subjects your physician can help you address that may be causing restlessness.
• Ear plugs can work wonders for people who are light sleepers.
5. Are you sleepy during the day?
This can be caused by the obvious – too little sleep at night, but it can also be caused by depression, anxiety, stress, and even boredom. Daytime sleepiness is a vicious fatigue/sleepiness cycle of being tired during the day, so you nap, then you cannot go to sleep at night, so you are sleepy the next day, etc, etc and the cycle continues.
Tip: The best way to stop this sequence of sleepiness during the day and not tired at night is to stay occupied during the day – go for a walk, meet up with friends, work on a hobby.
• Do not nap! This is easier said than done when you are dragging during the day, but in the long run, it helps you have a more restful night’s sleep, resulting in less daytime sleepiness.
6. Is pain a factor affecting sleep hygiene?
Pain and insomnia go hand in hand. – it triggers poor sleep, therefore, triggering more pain.
Tip: Consult your physician regarding uncontrolled pain. Many people use painkillers or sleeping pills to control insomnia, which can be effective, but prolonged use may not be the answer.
• Occupational or physical therapists use methods such as manual techniques, strengthening, and modalities such as heat and ice or addressing pain from a biopsychosocial model, and other modalities including relaxation and visualization activities.
• Have you considered consulting with a pain specialist? There may be ways to treat the pain, not mask it.
• Alternative medicine professionals? Massage, relaxation and breathing techniques have also been used as pain control methods.
7. When and how much do you use stimulants or depressants?
Caffeine in the form of soda, chocolate, coffee or tea too late in the day can prevent you from falling asleep effectively due to its stimulating nature. Alcohol can help you fall asleep, but it is common for it to awaken you after the alcohol metabolizes in your body during the second half of the night.
Prescription and over-the-counter medications can also have a great influence on sleep quality.
Tip: Cut out caffeine 3-4 hours before hitting the hay.
• Pay attention to how much alcohol you are consuming before bed – reduce or eliminate for a more restful night’s sleep.
• Look at the side effects of your prescription or over-the-counter medication – consult your physician to see if it can be taken at a different time of day or alternative medication options.
8. What environmental factors affect your nighttime sleep hygiene
habits?
Looking at where you drift off for the night is just as important as looking at the things that are going on around you.
- Are you sleeping in your own bed?
- Is it comfortable or do you need a new one?
- Have you thought about using pillows between your legs or a new pillow for better positioning?
- Is there a lot of noise in your bedroom?
- Is it too light?
Tip: If sleep is starting to truly impact your daily life, it is time to make sleep hygiene a priority!
- Try white noise machines, black out shades, eye masks or positioning pillows to increase your comfort.
Leave a comment below telling us your #1 tip.





2 thoughts on “8 Effective Tips for Sleep Hygiene in Occupational Therapy”
I often recommend clients use a heavy
(weighted) blanket to help calm the CNS before falling asleep. No need to buy one if you have wool blankets or heavy felt, such as horse blankets. Layering is recommended to find one’s ” sweet spot”. Caution required with children, however, as child should always be able to remove blanket independently, for safety. Deep pressure, generally, helps most people prepare for sleep.
Agreed – I love weighted blankets too!
I would also caution required for adults that cannot remove the blanket independently as well, such as people with dementia or physical limitations. Thanks for the recommendation Mary